What you should know about Lymphedema.
The following information is for people who have had mastectomies, lumpectomies, radiation treatment, lymph node removal, surgeries, or trauma to the limbs. You may be at risk for developing lymphedema. Or perhaps you or a family member were diagnosed at birth, during childhood or early adulthood with lymphedema. This information will help you understand what lymphedema is and how it can be managed.
“One day I awoke and my arm and hand were swollen. I thought I would just elevate it for awhile and the swelling would subside. Days later and much to my frustration, nothing happened. Little did I know, this was not going to be a temporary thing. What could it be? What caused this? What was I going to do? I want you to read on, knowing this information really saved my life.” – E.D.
If you know someone who may be at risk for developing lymphedema: Please be sure he or she reads this brochure and gives a copy to his or her doctor. Creating awareness and understanding about lymphedema is our goal.

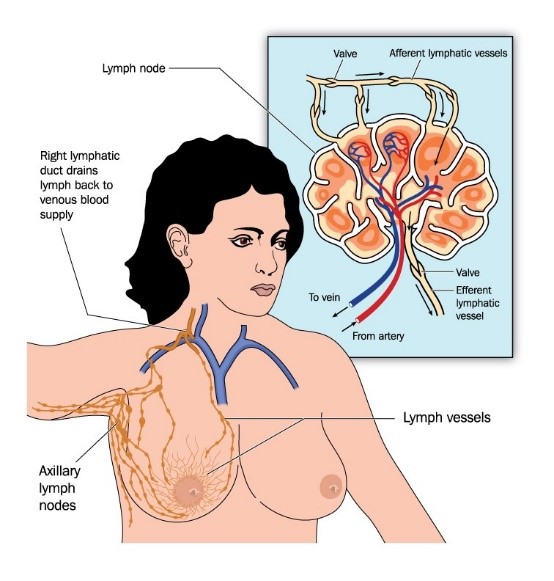
The Lymphatic system.
Your lymphatic system plays a large role in immune function and circulation. It consists of lymph vessels meeting up with lymph nodes located in your neck, armpits, and groin. As the lymph vessels move fluid out of the tissues, waste products, bacteria, dead cells, and large protein molecules are collected. The waste products are carried to the lymph nodes to be broken down and eliminated, while the protein rich fluid is transported back to the heart to rejoin circulation.
When the lymph vessels are unable to transport lymph fluid back into circulation it accumulates, resulting in chronic swelling. If left untreated it may result in hardening skin tissue. This build up of protein-rich lymph fluid is known as lymphedema. Once this condition occurs, the swelling may increase if an effective treatment program is not initiated.
How does Lymphedema Develop?
Lymphedema most often develops in one arm or leg, but may be present in both arms and both legs. It may also occur in the hands or feet, and even in the chest, back, neck, face, abdomen, and genitals.
Primary Lymphedema.
Primary Lymphedema is caused by malformations of the lymphatic system. These malformations are most common in women. Symptoms may be present at birth or may develop later, often during puberty or pregnancy. Primary lymphedema is most common in the legs, but may also occur in the arms or torso.
Secondary Lymphedema.
Secondary Lymphedema is a result of damage to the lymphatic system. Surgical procedures such as mastectomies, lumpectomies with radiation and/or removal of lymph nodes are the most common causes. Secondary lymphedema occurs most commonly in the arms, but may also develop in the legs. Other causes may include a traumatic injury, infection, or severe chronic venous insufficiency.

What are the symptoms?
Lymphedema may develop within a few months after a procedure, years later, or not at all. The first obvious sign of lymphedema is swelling characterised by “pitting”. This is recognisable when the skin is depressed for a few seconds and the indentation does not immediately disappear. Other symptoms may include a tightness or heaviness in the affected area or changes in the texture of the skin. You may even notice that jewellery and clothing feel tighter.
What to do if symptoms occur?
If you lymphatic system is compromised, this area of the body will have to work much harder to circulate fluid. When it is unable to keep up, swelling and fluid build-up are likely to occur. This is why the lymphatic vessels in the compromised area need external support.
Wearing a compression garment.
Wearing a compression garment provides external pressure to assist lymph drainage and hopefully prevent additional swelling. Although swelling is sometimes reversible, in most cases it is not and could lead to chronic lymphedema.
When you are about to engage in repetitive motions, such as exercise, cleaning, yard work, golfing or tennis it is a good idea to wear a compression garment. It is also important to wear a compression garment when you are flying. The decrease in cabin pressure in the airplane puts stress on the lymphatic and circulatory systems and this can increase swelling.
What is the treatment for lymphedema?
Once the diagnosis of lymphedema is confirmed, certain treatment procedures are indicated. Since there is no cure for lymphedema, the goal of treatment is to reduce swelling and to maintain the reduction. For a majority of patients, this can be achieved by the skilful application of Complete Decongestive Therapy (CDT) which is safe, reliable, and non-invasive. It is proven to provide positive long-term results for both primary and secondary lymphedema. CDT is performed by specially trained therapists. The treatment consists of four components:
- Manual Lymph Drainage (MLD)
- Graduated Compression Garments or bandages
- Meticulous Skin Care
- Therapeutic Exercises
Treatment.
Complete Decongestive Therapy works in two phases, the first being to move the lymph fluid out of the affected region and reduce the swelling using MLD techniques and bandaging. Ideally these treatments are performed daily, five days a week for 2-4 weeks, depending on the severity. Once the swelling is reduced, the patient is fitted with a graduated compression garment. This marks the second phase, in which the patient plays a large role in his or her ongoing self-care. Wearing graduated compression garments, being meticulous about skin care, and performing self-manual lymph drainage and therapeutic exercises will assure continued success.
Treatment procedures such as diuretics or surgery are not appropriate for lymphedema. Initially, a diuretic will decrease the water content and reduce swelling, but the protein molecules remain in the tissues and swelling will reoccur as soon as the drug loses its effectiveness. Surgical methods for lymphedema have not proven successful.
“Its important to be consistent in wearing your garment.” McKenna Johnson, lymphedema patient and long-time Juzo customer.

A closer look at the treatment.
Manual Lymph Drainage (MLD):
Manual Lymph Drainage is necessary to manage fluid volume of the affected extremity to a normal or near normal size. Bandages are used in the phase 1 and compression garments in phase 2.
Graduated Compression Garments:
Graduated compression garments are necessary to maintain the reduced limb and are designed to replace the bandages that were used earlier in treatment. They are worn during the day while you are active. At night when you sleep, bandages or night garments are usually worn. The compression garments help to keep the swelling down, improve circulation, and prevent the reaccumulation of lymph fluid in the area. The garments must be worn everyday, for life.

Pneumatic Compression Pumps:
Some treatments may include use of a pneumatic compression pump. This mechanical device works as a sleeve with chambers that are intermittently inflated with air. This device is sometimes used in combination with CDT.
Skin Care:
With lymphedema, the skin is usually dry and may crack easily, making it very susceptible to infections. A low-pH lotion, free of alcohol and fragrances should be used to maintain the moisture of the skin and to protect it. If an infection develops, consult your physician immediately!
Exercise:
A skilled therapist may recommend an exercise program that is suited for your particular need and ability. An effective decongestive exercise program aids the muscular system to move lymph fluid out of the affected area. Any exercise that causes pain or muscle soreness should be discussed with a therapist. Moderate exercise such as swimming, walking, biking, light weight training and yoga are recommended. Overly aggressive sports that may cause injury should be avoided. Consult your physician before beginning and program.

Lifestyle.
Tips for managing and living with lymphedema.
If you are at risk for developing lymphedema or already have it, these guidelines will help you prevent and manage the condition. Although you may not need to follow each suggestion, it is good to be aware of them.
If you have lymphedema, it is important that you avoid injury and overexertion in the affected area. You should wear the prescribed compression garments and/or bandages as instructed by your physician or therapist. Be sure all of your medical charts are updated and consider wearing a lymphedema alert bracelet available through the National Lymphedema Network.
Clothing and Jewellery.
Avoid tight or restrictive clothing that may impair circulation or cause irritation and swelling. Shirt sleeves, bra straps, belts, socks, and shoelaces should fit comfortably. Shoes with low heels are recommended. Jewellery, including watches, bracelets, and rings should not feel tight. Avoid carrying heavy purses, luggage and shoulder bags on the side that is affected.
Skin Care.
Keep skin protected using moisturising lotion and wash with a mild pH balanced soap. When bathing, water should be warm, not hot. Avoid irritating or allergy-causing cosmetics, detergents, deodorants, and perfumes. Inspect your feet, hands, and limbs regularly for skin changes since open skin invites bacteria and infection. Avoid cuts, pricks, scratches, burns, and insect bites that could increases swelling or promote infection. Use sunscreen and insect repellent regularly. Gloves are also a good protective measure for the hands when washing dishes, cooking, cleaning or working outdoors.
Trauma can also increase swelling and further damage the lymphatic system: Avoid blood pressure checks, IV’s, blood draws, and shots in the affected limb. Do not cut into the cuticles when trimming fingernails or toenails. Use an electric razor when shaving.
Proper Nutrition.
Increased weight complicates lymphedema. Maintain a balanced diet of fruit, vegetables, whole grains and protein. Avoid excessive consumption of fatty foods, sweets, salt and alcohol. Drink plenty of water and unsweetened liquids.
Exercise.
Moderate exercise such as swimming, walking, biking, light strength training and yoga are recommended. Overly aggressive sports that may cause injury should be avoided. Consult your physician before beginning any program.
Weather and traveling.
Always wear compression garments when flying or driving, as recommended by your physician or therapist. When travelling by car, be sure the seatbelt is comfortable and make frequent stops since prolonged sitting may increase swelling. Avoid extreme changes in temperature (over 90 degrees or below zero), sun bathing, tanning beds, saunas, steam rooms, and hot tubs.

FAQs
Will lymphedema ever go away?
If it is diagnosed early, lymphedema can be managed through proper treatment, quality of compression garments, and good skin care. That is why management is key.
Where do I find an MLD therapist?
Many hospitals have trained MLD therapists in their physical and occupational therapy department or outpatient rehabilitation centres. Lymphedema organisations list MLD therapists on their websites. NALEA (North American Education Services) – www.lymphedemaeducationassociation.org
Where can I buy compression garments?
Compression garments are sold at medical supply stores and some pharmacies. Measurements are taken by a certified fitter to ensure garments fit properly. Go to juzosa.com to find a local dealer.
Will my insurance pay for compression garments?
That depends on what type of insurance you have and what state you live in. Call your insurance company to verify coverage.
How do I care for my compression garments?
Daily machine wash and dry with a mild detergent is recommended to maximise therapeutic effectiveness. Do not use fabric softeners, chlorine or bleach which may damage your garment. Refer to the manufacturer’s care instructions.
How do I put compression garments on?
Wearing donning gloves is recommended to protect your garments from fingernail and jewellery snags. There are also numerous assistive devices that make putting on and taking off garments easy and comfortable. Ask your certified fitter for a demonstration of these devices.
Garments.
Juzo offers a complete line of compression products for lymphedema management. From compression stockings to arm sleeves, and other gauntlets, Juzo garments are comfortable, durable and fashionable. They provide therapeutic compression and have many added value features and benefits. Garments will maintain their compression for six months.

“I bought one pair to try and fell in love… and can’t stop bragging about them and showing them off. Within one week of wearing them my legs felt better and looked better! It is a wonderful feeling to be ‘normal’ again!” – HRBS
“After breast cancer, I was told that I had lymphedema and the best garments to wear are Juzo, that I would enjoy the comfort, fit, and flexibility. And after wearing ten sleeves and gloves in the last three years, I am truly happy. Juzo has made lymphedema much more manageable. Thank-you.” – Brenda D
“I am using your arm sleeve for two years with excellent results. I think your product is very comfortable and makes my life so easy! Thanks.” – Maria J
“I have found with lymphedema, that my patients have had more success and comfort with Juzo as compared to (competitors). I, as a physical therapist, have been very satisfied with the product line.” – Jamie D, Physical Therapist.
